by, Marko Vujicic, PhD and Chelsea Fosse, DMD, MPH
Dental care services have a long history of being financed and delivered separately from medical care services. Dating back to the mid-1800s, dental schools and associations were established independently of medical schools and associations. Regrettably, several important US health care reform milestones have reinforced this separation—most recently, the Affordable Care Act (ACA) of 2010.
Under the ACA, dental care for adults was not included as an essential health benefit, and, while dental care for children was included and lowered total financial outlays, the increase in stand-alone dental plans between 2014 and 2016 reinforced the separation of dental and medical insurance.
What are the implications of financing and delivering dental care separately from medical care? We pose pose some key questions for policymakers seeking to address these issues.
Oral Health Inequity
Improvements in the oral health of the US population vary by age, income, and racial or ethnic group. Among children, disparities by race and income are narrowing for many oral health indicators. For example, children from low-income families and Black and Hispanic adults are more likely to have untreated tooth decay, but children and adolescents from low-income families and Black and Hispanic children ages 6 and older have seen the biggest improvements in recent years.
Among seniors, untreated cavities are far more common in Black and Hispanic populations. Another important outcome, retention of natural teeth, highlights the disparities that exist among older adults. While older Americans in general are retaining more teeth than in the past, the improvements have mainly occurred among high-income seniors. In other words, income inequity is widening when it comes to retaining your natural teeth.
Oral health improvements occur for many reasons, including better access to dental services. Recent data show that working-age adults and seniors are more likely to face financial barriers to obtaining needed dental care than children. Dental care utilization trends have been driven in large part by trends in dental insurance coverage. In 2015, 10% to 12% of US children were uninsured for dental care services compared to 28% of working-age adults and 62% of seniors. The share of US children with some form of dental insurance has increased significantly in the past 2 decades, from 73% in 1996 to 88% in 2015, with the most significant gains in dental insurance coverage being among children from low-income families. Among working-age adults and seniors during the same period, dental insurance coverage rates increased modestly, from 67% to 72% for the former and from 35% to 38% for the latter.
Public Policy
For children from low-income families enrolled in Medicaid, dental insurance coverage is guaranteed by the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. This mandatory benefit requires that the Medicaid program and the Children’s Health Insurance Program (CHIP) provide comprehensive, medically necessary dental services to all children under age 21. Roughly 43% of general practice dentists participate in Medicaid or CHIP for child dental services. While dentist participation in Medicaid is much lower than physician participation, the available evidence suggests that financial issues or lack of prioritization of dental care are key barriers to dental care for children as well.
Dental insurance for adults at all income levels, on the other hand, is not guaranteed. Adult dental benefits under state Medicaid programs are optional, and there is significant state-to-state variation in terms of what dental services are covered. According to the most recent analysis, 3 states provide no adult dental benefits, 10 states provide emergency-only benefits, 16 states provide limited benefits, and 20 states cover a more comprehensive mix of dental services. Medicare, the medical insurance program for adults ages 65 and older, does not cover routine dental services. However, roughly 94% of Medicare Advantage (Part C) enrollees in individual plans had some dental services included as a part of their benefits package in 2021.17
Between 2000 and 2015, dental benefits utilization and insurance coverage of dental services for children increased,18, 19 reducing oral health inequity among children from families with low-income and among Black and Hispanic children.7 But inequity has not decreased for working-age adults and seniors. Why does age alone dictate whether society deems oral health essential? Different policy approaches to dental insurance for children, working-age adults, and seniors affect affordability. For all age groups, data suggest that financial barriers to dental care are more significant than for any other health service,20 yet children face dramatically lower financial barriers to dental care than working-age adults and seniors (see Figure).20
Figure. Financial Barriers to Dental Care and Other Types of Health Care Services in 2019
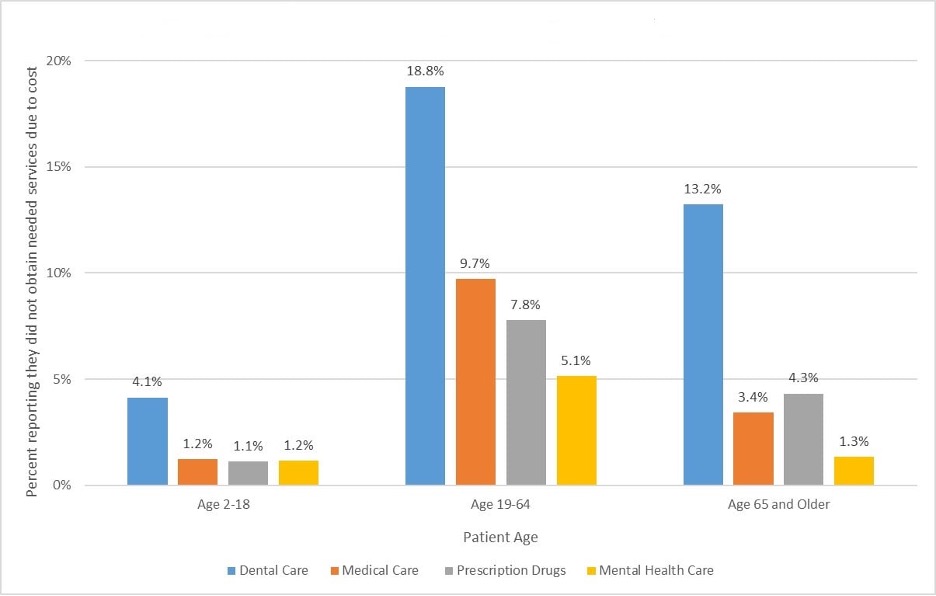
a Data from National Center for Health Statistics.21
Even when dental coverage is offered, it is almost always as a stand-alone dental plan (SADP) and not embedded as part of a medical plan. Among the privately insured prior to the passage of the ACA, 99% of those with dental insurance obtained that coverage through SADPs. (As of 2017, the take-up rate of SADPs in federally facilitated marketplaces was only 16% for adults and 17% for children.) Moreover, Medicaid dental programs are administered separately from medical programs, with different provider network arrangements, different patient record systems, and different care coordination challenges for clinicians.23, 24 Thus, affordability challenges for working-age adults and seniors aside, dental care delivery is not effectively linked with medical care delivery in the true sense of a health care “system.”
For all age groups, data suggest that financial barriers to dental care are more significant than for any other health service.
System fragmentation undermines medical-dental care coordination. Physicians’ referrals to dentists are compromised by separate insurance systems and lack of service delivery integration. Moreover, accountable care organizations tend not to offer dental services due to coverage gaps in their patient base and practical challenges posed by differences in information technology platforms used by medical and dental clinicians.26
What Now?
In our view, the income, age, and race inequity in oral health outcomes, dental care use, and affordability stem from major dental insurance coverage gaps for vulnerable populations and lack of medical-dental integration that would facilitate interprofessional referrals and care. Current dental care financing and delivery streams leave vulnerable groups behind. We urge policymakers and stakeholders to consider 2 key policy questions.
Should dental care be considered an essential health care service for people of all ages within public and private insurance programs? Medicaid’s EPSDT benefit has proven effective in improving oral health outcomes and reducing inequity among children. This policy approach can be used to design and implement similar mandatory dental benefits for adults.
In January 2021, Congress introduced the Medicare Dental Benefit Act of 2021, which calls for inclusion of oral health benefits in Medicare Part B for the two-thirds of Medicare beneficiaries who currently have no dental coverage. Expanding dental coverage to adults and seniors would likely reduce costs for those with chronic health conditions (eg, diabetes), improve oral health and well-being, and promote economic productivity among working-age adults.
What is needed to improve care coordination between medical and dental practitioners? There are 27 million people who visit a dentist but not a physician and 108 million who visit a physician but not a dentist in any given year. There are undoubtedly medical and dental conditions going undetected in these respective populations that, if addressed, would improve overall health and potentially reduce long-term health care costs.
Current dental service delivery streams do not enable effective care coordination between dental practitioners and other clinicians. Foundational changes in education and training programs are needed to facilitate interprofessional patient care. Diagnostic data is not collected routinely in dental insurance data. Dental insurers must recognize the importance of coding procedures and diagnoses to track outcomes and contribute to evidence-based practice. Integrated health information technology and enhanced understanding of the day-to-day care offered by medical colleagues would facilitate referral processes and increase access to care.
Act Now
Former US Surgeon General David Satcher said more than 20 years ago that “you cannot be healthy without oral health.” Certainly, we have made progress in improving oral health for children since then, especially for vulnerable children. But for working-age adults and seniors, disparities in oral health outcomes and in access to dental care have widened by income and race. Treating dental care as essential in US health policy—for all ages, not just children—is the only way to address these challenges.
REFERENCES
- Simon L. Overcoming historical separation between oral and general health care: interprofessional collaboration for promoting health equity. AMA J Ethics. 2016;18(9):941-949.View ArticlePubMedGoogle Scholar
- Mertz EA. The dental-medical divide. Health Aff (Millwood). 2016;35(12):2168-2175.View ArticlePubMedGoogle Scholar
- Vujicic M, Yarbrough C. Estimating premium and out-of-pocket outlays under all child dental coverage options in the federally facilitated marketplace. J Pediatr. 2017;182:349-355e.1.View ArticlePubMedGoogle Scholar
- Nasseh K, Vujicic M. Dental plan premiums in the Affordable Care Act marketplace trended downward from 2014 through 2016. J Am Dent Assoc. 2017;148(4):230-235.View ArticlePubMedGoogle Scholar
- Gupta N, Vujicic M, Yarbrough C, Harrison B. Disparities in untreated caries among children and adults in the US, 2011-2014. BMC Oral Health. 2018;18:30.View ArticlePubMedGoogle Scholar
- Hinton E, Paradise J. Access to dental care in Medicaid: spotlight on nonelderly adults. Kaiser Family Foundation. March 17, 2016. Accessed February 26, 2021. https://www.kff.org/medicaid/issue-brief/access-to-dental-care-in-medicaid-spotlight-on-nonelderly-adults/
- Lin M, Griffin SO, Gooch BF, et al. Oral health surveillance report: trends in dental caries and sealants, tooth retention, and edentulism, United States, 1999-2004 to 2011-2016. Centers for Disease Control and Prevention; 2019. Accessed February 26, 2021. https://www.cdc.gov/oralhealth/pdfs_and_other_files/Oral-Health-Surveillance-Report-2019-Web-h.pdf
- Dye BA, Weatherspoon DJ, Lopez Mitnik G. Tooth loss among older adults according to poverty status in the United States from 1999 through 2004 and 2009 through 2014. J Am Dent Assoc. 2019;150(1):9-23.e3.View ArticlePubMedGoogle Scholar
- Crall JJ, Vujicic M. Children’s oral health: progress, policy development, and priorities for continued improvement. Health Aff (Millwood). 2020;39(10):1762-1769.View ArticlePubMedGoogle Scholar
- Gupta N, Vujicic M; Health Policy Institute. Main barriers to getting needed dental care all relate to affordability. American Dental Association; April 2019.Google Scholar
- Manski RJ, Rohde F. Research findings #38: dental services: use, expenses, source of payment, coverage and procedure type, 1996-2015. Agency for Healthcare Research and Quality; 2017. Accessed February 26, 2021. https://meps.ahrq.gov/data_files/publications/rf38/rf38.shtml#Findings
- Yarbrough C, Reusch C. Progress to build on: recent trends on dental coverage access. Children’s Dental Health Project blog. October 18, 2018. Accessed February 26, 2021. https://www.cdhp.org/blog/557-progress-to-build-on-recent-trends-on-dental-coverage-access
- Early and periodic screening, diagnostic, and treatment. Medicaid.gov. Accessed February 26, 2021. https://www.medicaid.gov/medicaid/benefits/early-and-periodic-screening-diagnostic-and-treatment/index.html
- Health Policy Institute. Dentist participation in Medicaid or CHIP. American Dental Association; August 2020.Google Scholar
- Health Policy Institute. Medicaid fee-for-service (FFS) reimbursement and provider participation for dentists and physicians in every state. American Dental Association; April 2017.
- Center for Health Care Strategies. Medicaid adult dental benefits coverage by state. September 15, 2019. Accessed August 16, 2021. https://www.chcs.org/media/Medicaid-Adult-Dental-Benefits-Overview-Appendix_091519.pdf
- Freed M, Ochieng N, Scroczynski N, Damico A, Amin K. Medicare and dental coverage: a closer look. Kaiser Family Foundation. July 28, 2021. Accessed October 5, 2021. https://www.kff.org/medicare/issue-brief/medicare-and-dental-coverage-a-closer-look/
- Health Policy Institute. Dental care utilization in the US. American Dental Association; November 2017.
- Health Policy Institute. Dental benefits coverage in the US. American Dental Association; November 2017.Google Scholar
- Vujicic M, Buchmueller T, Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff (Millwood). 2016;35(12):2176-2182.View ArticlePubMedGoogle Scholar
- National Center for Health Statistics. 2019 National Health Interview Survey. Centers for Disease Control and Prevention. Reviewed April 5, 2021. Accessed February 26, 2021. https://www.cdc.gov/nchs/nhis/2019nhis.htm
- Regulatory treatment of pediatric dental coverage outside exchanges. National Association of Dental Plans. May 2015. Updated July 2, 2015. Accessed February 24, 2021. https://www.nadp.org/docs/default-source/hcr-documents/issue-brief_may2015_v4.pdf?sfvrsn=2
- Health Policy Institute. 2017 take-up rate of stand-alone dental plans. American Dental Association; May 2017.
- Manski RJ, Hoffmann D, Rowthorn V. Increasing access to dental and medical care by allowing greater flexibility in scope of practice. Am J Public Health. 2015;105(9):1755-1762.View ArticlePubMedGoogle Scholar
- Atchison KA, Rozier G, Weintraub JA. Integration of oral health and primary care: communication, coordination, and referral. NAM Perspect. October 8, 2018. Accessed November 16, 2021. https://nnoha.org/nnoha-content/uploads/2019/12/Integration-of-Oral-Health-and-Primary-Care.pdf
- Leader D, Vujicic M, Harrison B; Health Policy Institute. Could dentists relieve physician shortages, manage chronic disease? American Dental Association; December 2018.Google Scholar
- Vujicic M. Our dental care system is stuck. And here’s what to do about it. J Am Dent Assoc. 2018;149(3):167-169.View ArticlePubMedGoogle Scholar
- Medicare Dental Benefit Act of 2021, HR 502, 117th Cong (2021). Accessed February 26, 2021. https://www.congress.gov/bill/117th-congress/house-bill/502?s=1&r=28
- Freed M, Neuman T, Jacobson G. Drilling down on dental care coverage and costs for Medicare beneficiaries. Kaiser Family Foundation. March 13, 2019. Accessed August 30, 2021. https://www.kff.org/medicare/issue-brief/drilling-down-on-dental-coverage-and-costs-for-medicare-beneficiaries/
- Freed M, Potetz L, Jacobson G, Neuman T. Policy options for improving dental coverage for people on Medicare. Kaiser Family Foundation. September 18, 2019. Accessed February 26, 2021. https://www.kff.org/medicare/issue-brief/policy-options-for-improving-dental-coverage-for-people-on-medicare/
- Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med. 2014;47(2):166-174.View ArticlePubMedGoogle Scholar
- Health Policy Institute. Oral health and well-being in the United States. American Dental Association; 2015. Accessed February 26, 2021. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/us-oral-health-well-being.pdf
- US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. Accessed November 8, 2021. https://www.nidcr.nih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf
AUTHOR INFORMATION
- Marko Vujicic, PhD is chief economist and vice president of the Health Policy Institute of the American Dental Association in Chicago, Illinois, which collects and analyzes data on practice consolidation trends, oral health outcomes, the dental workforce, dental education, and dental benefits. Formerly, he was an economist with the World Bank and the World Health Organization.
- Chelsea Fosse, DMD, MPH is a senior health policy analyst with the Health Policy Institute of the American Dental Association in Chicago, Illinois. She earned an DMD degree from Rutgers School of Dental Medicine and an MPH degree from the Mailman School of Public Health at Columbia University. Her research centers on policy issues related to Medicaid, Medicare, public health, the Affordable Care Act, and other public policy issues.